Curing African Sleeping Sickness with a Biochemical Trojan Horse
Posted on January 19, 2024 • 3 minutes • 453 words
Table of contents
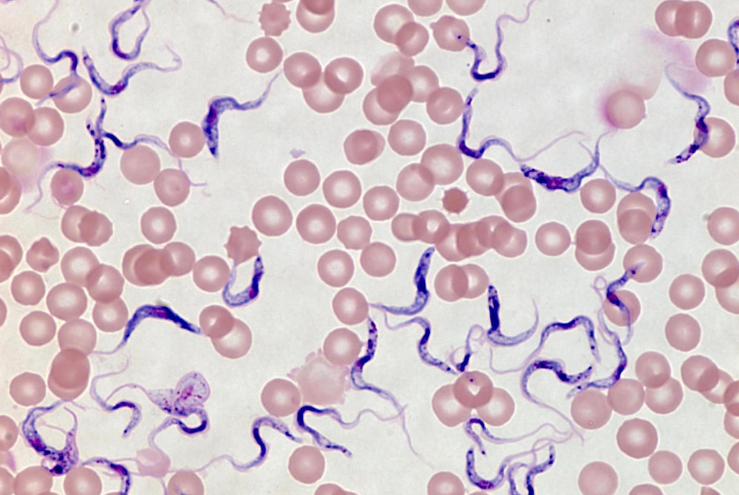
African sleeping sickness, also known as African trypanosomiasis, is a disease triggered by single-celled eukaryotes known as trypanosomes. This illness, along with other diseases caused by trypanosomes, holds significant medical and economic impact in numerous developing countries. Historically, until the late 20th century, it was almost untreatable, with vaccines proving ineffective due to the parasite’s unique ability to bypass the host’s immune defense.
The surface of trypanosome cells is coated with a single type of protein, which acts as the antigen triggering the human immune response. Periodically, through genetic recombination, some trypanosome cells alter their protein coat, rendering them unrecognized by the immune system. This “coat switching” can happen repeatedly, leading to a prolonged, cyclical infection. Initially, the host experiences fever, which diminishes as the immune system counters the initial wave of infection. However, trypanosomes with new coats trigger subsequent infections, causing recurring fevers. This ongoing cycle can continue for weeks, eventually leading to the host’s death due to the persistent weakening of their health.
| Tse-Tse fly |
|---|
 |
A strategy to combat African sleeping sickness involves the use of pharmaceuticals designed as mechanism-based enzyme inhibitors, specifically targeting the trypanosomes' polyamine biosynthesis pathway. Polyamines like spermine and spermidine, essential for DNA structuring, are in high demand in fast-dividing cells. The first step of their synthesis involves ornithine decarboxylase, an enzyme dependent on a coenzyme named pyridoxal phosphate (PLP). PLP, derived from vitamin B6, forms a covalent bond with amino acid substrates, aiding various reactions. Unlike in mammalian cells where this enzyme is rapidly replaced, in certain trypanosomes, it remains stable and not easily substituted. Thus, an inhibitor that permanently binds to this enzyme can significantly impair the parasite while minimally affecting human cells, which can quickly regenerate the inhibited enzyme.
The inactivation process involves CO release, reversing electron movement and leading to putrescine production. Based on this mechanism, various suicide inhibitors have been created, including difluoromethylornithine (DFMO). Inactive in solution, DFMO rapidly incapacitates ornithine decarboxylase upon binding. It functions by offering an alternative electron sink with two strategically positioned fluorine atoms, excellent leaving groups. The reaction diverts electrons away from PLP’s ring structure, resulting in a fluorine atom’s displacement. A Cys residue at the enzyme’s active site then forms a stable covalent complex with the reactive PLP-inhibitor adduct. This process leverages the enzyme’s own mechanisms for its inactivation.
DFMO has shown high efficacy in treating African sleeping sickness caused by Trypanosoma brucei gambiense. Such methods hold significant potential for treating a variety of diseases, illustrating the promise of drug design based on enzyme mechanism and structure, a supplement to traditional trial-and-error pharmaceutical development approaches.
References
Share
Tags
Counters